 |
 |
AbstractOnodi cell sinusitis is a rare cause of isolated oculomotor nerve palsy. The sphenoid sinus and Onodi cell mucocele or invasive fungal sinusitis are often associated with multiple cranialnerve symptoms simultaneously. However, isolated cranial nerve palsy due to simple sinusitis is rare. Sinus disease associated with cranial nerve palsy is difficult to diagnose based on patient history or physical examination alone; CT and MRI help in correctly assessing these lesions. Here we report a case of Onodi cell sinusitis observed in a patient who presented with isolated oculomotor nerve palsy. The patient underwent endoscopic sinus surgery and recovered completely at 2 months postoperative.
IntroductionSinusitis occurs widely at any age, regardless of sex or race, and chronic sinusitis has a prevalence of 1%-12%, according to diagnostic criteria[1]. The main symptoms of sinusitis include nasal congestion, rhinorrhea, decreased sense of smell, and facial discomfort. However, sinusitis is a heterogeneous inflammatory disease that sometimes shows unique symptoms without the above-named cardinal symptoms.
In particular, rhinologic symptoms do not often appear in the case of the posterior sinus involvement, while unusual symptoms such as headache or visual symptoms appear [2]. Thus, the clinician sometimes misdiagnoses or delays treatment. The structures adjacent to the posterior sinus, such as the optic nerve, internal carotid artery, and cavernous sinus, are affected, and mortality rate of 2.9% has been reported [3].
Onodi cells, located laterally and superiorly into the sphenoid sinus, may often aerate the anterior clinoid process (ACP). Onodi cells and the aerated ACP are also in contact with important structures, and neurological symptoms due to inflammation and tumors of these structures have been reported [4]. Since sinusitis is not common as a cause of isolated cranial palsy, it is easy to overlook it unless sufficient suspicion is preceded [5].
We report the case of one patient with Onodi cell sinusitis with isolated oculomotor nerve palsy who underwent endoscopic sinus surgery and recovered completely after 2 months.
CaseA 75-year-old male patient visited our neurology department with persistent double vision and headache for 3 days. The patient had a history of hypertension and diabetes. Physical examination revealed that the right ptosis and exotropia of the right eye. Visual acuity and intraocular pressure were normal, and no abnormalities were observed in bilateral pupil control. In the extraocular muscle examination, there was a complaint of horizontal diplopia between 45 degrees to the right and 180 degrees to the left during binocular gaze and adduction, supination, and downward restriction of the right eye, and worsening on left gaze (Fig. 1).
There were no significant abnormalities in laboratory test except HbA1c, slightly increased to 7.2. On the day of admission, brain MRI showed past lacunar cerebral infarction but no lesions in the brain parenchyma that could explain the symptoms were observed. On the right Onodi cell and ACP, brain MRI showed intermediate on T1, intermediate to low signal on T2, enhanced mucosa on the peripheral wall in gadolinium imaging and extraconal haziness were found (Fig. 2A-D). Compared with the normal left side, the right oculomotor nerve was compressed due to peripheral edematous changes (Fig. 2E). Also, there was a slightly low signal and some heterogeneous contrast enhancement on the T1- and T2-weighted images on the right posterior ethmoid sinus. A disease such as fungal sinusitis had to be differentiated. However, sinus lesions were not recognized at the time of imaging in the neurology department, and steroid pulse therapy (methylprednisolone 1000 mg qd) was maintained for 3 days.
On the third day of hospitalization, the radiology department requested to collaborate with the otolaryngology department about the lesion on the Onodi cell. No rhinologic symptoms such as rhinorrhea, nasal obstruction, or hyposmia were reported; the endoscopic examination showed slightly swollen mucosa without purulent rhinorrhea. On the fourth day of hospitalization, paranasal sinus CT was taken. Compared with the MRI taken 3 days before, the lesion filled with Onodi cells and ACP was reduced, and there were erosions in the Onodi cell walls but no bony defect (Fig. 3). It was thought that the sinus lesion caused the nerve palsy, so an intravenous (IV) antibiotic injection (levofloxacin 500 mg qd) was started, and the emergent operation was performed on the same day.
Under general anesthesia, fronto-maxillo-ethmoidectomy was done. Onodi cells were removed, and the natural foramen was widened sufficiently. Severe edema of the mucosa around the opening of the Onodi cell was found (Fig. 4A). Onodi cells were filled with thick mucus secretion and were removed, and there were no defects in the inner optic nerve canal or cranial base (Fig. 4B). Permanent pathology showed chronic inflammation. After surgery, the patientŌĆÖs discomfort of moving the eyeball decreased, but diplopia still remained. After IV antibiotic maintenance for 3 days, oral antibiotics (cefditoren, roxithromycin for 2 weeks), and steroids (prednisolone 10 mg maintained for 1 month) are maintained after surgery. The patient was discharged on the 5th day after surgery. Periodic follow-up was performed simultaneously at the departments of ophthalmology and otolaryngology. On the 20th day after surgery, ptosis was relieved and exotropia was partially resolved. Therefore, the steroid dose was gradually reduced and maintained for 1 month. At the postoperative 2-month follow-up, previously observed ptosis and exotropia were completely resolved (Fig. 5C), and no sinus lesions were observed on CT (Fig. 5A and B).
DiscussionConsidering that the lesions of the Onodi cell and ACP are similar to those of the sphenoid sinus, it can be expected that their pathophysiology will be similar. Because the anatomical barrier of the posterior sinus is weak and the bone layer of the sphenoid sinus is thin, it easily spreads when inflamed, showing various symptoms related to surrounding important structures [6]. In particular, when there is a correlation between cranial and ocular complications, it should be actively treated and not underestimated. Onodi cells are located at the back of the ethmoid sinus cells and are located laterally and superiorly to the sphenoid sinus. During normal growth, ethmoid sinus cells expand into the sphenoid sinus, causing failure of the sinus wall or creating an intracranial connection. Clinically, when the optic nerve and the internal carotid artery are located inside the cells, caution is required during surgery. The prevalence varies greatly, and it has been reported to vary from 12.7% to 47.3% in a study involving Koreans [7]. Although the prevalence of Onodi cell sinusitis is not known in detail, in the case of sinusitis confined to the sphenoid sinus in a similar location, it has been reported to be about 1% to 2.7% of all sinusitis [8].
Although there are cases of pus or postnasal drip in the sphenoethmoidal recess or nasopharynx through endoscopic examination, there are many cases with normal findings. If posterior cell sinusitis is suspected, diagnosis through imaging is required, and CT is the most useful. MRI can be used in cases of decreased visual acuity or cranial nerve palsy or to differentiate other pathologies such as mucocele, benign tumors, cerebral aneurysms, and internal carotid aneurysms [9].
The relationship between sinus disease and cranial nerve palsy is frequently observed in neoplastic and malignant tumors, but it has been reported in 12% of sinus inflammatory diseases [10]. When looking at cases of cranial nerve palsy related to sphenoid sinusitis, the most common was the 6th nerve palsy, followed by the 3rd nerve palsy [11]. The reason is thought to be that the 6th nerve is long and is located closest to the sphenoid sinus on the medial side of the cavernous sinus [2]. However, it is the 3rd nerve, not the 6th nerve, that runs closest to the ACP and the cavernous sinus. Hopf-Jensen, et al. [12] reported a case of 3rd nerve compression by a mucocele of the ACP. They believed that the oculomotor nerve palsy arose because the 3rd nerve was closest to the mucocele. And in our case, the symptoms arose because of the compression of the 3rd nerve due to inflammation of the ACP. In the cavernous sinus, the 3rd nerve passes closest to the inferolateral side of the ACP, so it is thought that it will be invaded more easily than other extraocular cranial nerves when the ACP is inflamed (Fig. 6) [13].
Treatment to prevent complications of sinusitis is broadspectrum antibiotic therapy. Surgery should be considered if there is no improvement or worsening within 24 to 48 hours or if diagnosed as fungal or mucocele. Even when the neurological symptom occurs, immediate surgery is required to restore nerve function [9]. Moreover, active drainage should be considered if a sinus lesion is found in a patient with ocular symptoms. In our patient, the Onodi cells were inflamed in the ACP, and 3rd nerve palsy occurred. MRI confirmed partial compression of the 3rd nerve in the cavernous sinus. As a mechanism of nerve paralysis, it is thought that temporary compression of the 3rd nerve caused the symptoms by direct compression due to sinus lesions or inflammatory edema change to surrounding tissues through bone erosion.
The main causes of isolated 3rd nerve palsy include microvascular ischemia, trauma, compression due to mass and iatrogenic [5]. As there are various causes, treatment must correct each cause, and the overall recovery rate is 48.3%-70.3%. With the emergent surgical drainage, using systemic steroids is important in cranial nerve palsy because it relieves symptoms by regulating the substances related to the immune response and reducing edema near the nerves [14]. It took quite a while to recover completely in this case. Possible causes are as follows: First, early intervention was delayed because the possibility of sinusitis was overlooked. The optimal treatment time for isolated 3rd nerve palsy is not known. However, El Mograbi and Soudry [11] analyzed 17 cases of isolated ocular nerve palsy caused by sphenoid sinusitis, and reported that surgery was performed within an average of 2.5 days after symptom onset, and complete recovery was usually achieved within 1 month [11]. In our patient, surgical treatment was performed 1 week after the onset of symptoms, and the recovery period was 2 months. We believe that the rather late treatment may have affected the recovery period. Second, surrounding cytokine release with edematous mucosa around the nerve can delay relieving cranial nerve symptoms.
In this case, we treated a patient who developed isolated 3rd nerve palsy due to inflammation of the Onodi cell and APC found on MRI. Since cranial nerve palsy is not a common complication of sinusitis, if it is overlooked, the diagnosis may be delayed, leaving fatal complications. Considering various symptoms, recognition through imaging tests for early diagnosis and rapid and active treatment will have an important influence in determining treatment policy.
ACKNOWLEDGMENTSThis work was supported by a faculty research grant of Yonsei University Wonju College of Medicine for 2022-52-0054 (granted to E.J.L.).
NotesAuthor Contribution Conceptualization: Cheol Hyo Ku. Data curation: Minheon Kim. Supervision: Eun Jung Lee. Visualization: Cheol Hyo Ku, Minheon Kim. WritingŌĆöoriginal draft: Cheol Hyo Ku. WritingŌĆöreview & editing: Dong-Joon Park, Eun Jung Lee. Fig.┬Ā1.Preoperative eyeball position. Limitation of right eyeball movement, including adduction, elevation, and depression. In primary gaze, upper lid ptosis and exotropia of the right eye were seen. Pupils are equal in size and reactive, with no relative afferent pupillary defect. 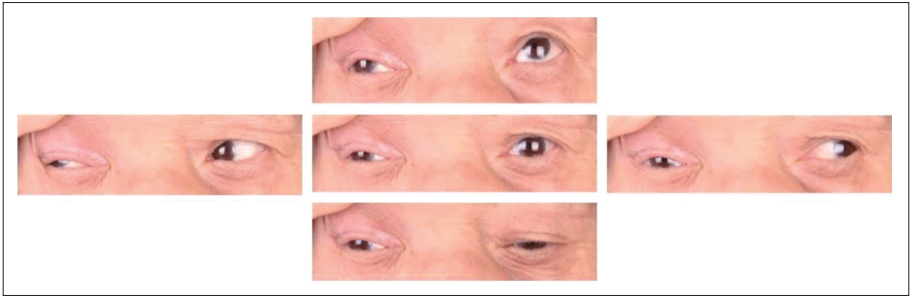
Fig.┬Ā2.Brain MRI. A and B: Preoperative MRI shows opacification on the Onodi cell, with intermediate signal on T1 image (A) and intermediate to low signal intensity on T2 flair image (B). C: Enhanced T1 image axial scan shows involved adjacent pneumatized anterior clinoid process (wide arrow) and some heterogeneous enhancement on posterior ethmoid mucosa with suspicious haziness on the extraconal area (thin arrow). D: T1 enhanced coronal scan shows an opacified and obstructed right Onodi cell. E: T1 enhanced coronal scan at the level of cavernous sinus shows some enhancement on the right side and 3rd nerve compressed by surrounding edema (thin arrow). Otherwise left oculomotor nerve shows normal anatomy (wide arrow). 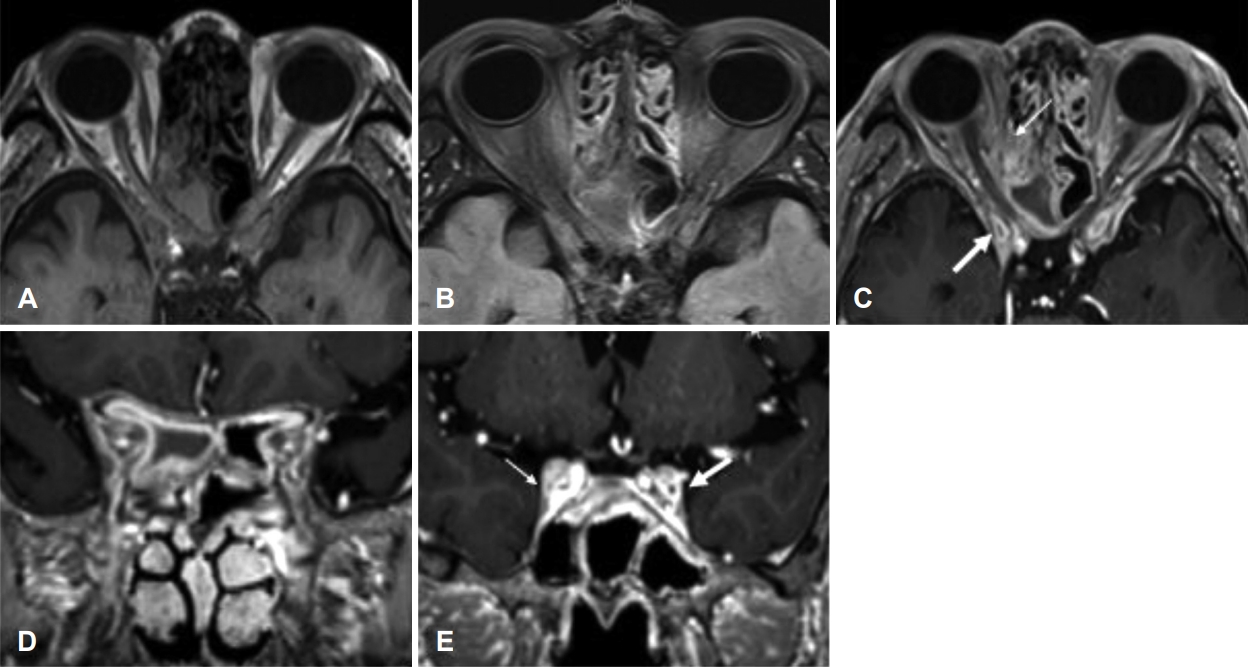
Fig.┬Ā3.Preoperative paranasal sinus CT. A: Axial scan shows partial opacification on the right sphenoethmoidal cell. B: Coronal scan shows diminished opacification on the anterior clinoid process compared to previous MRI scans and erosion on cell walls (arrows), but no prominent dehiscence. 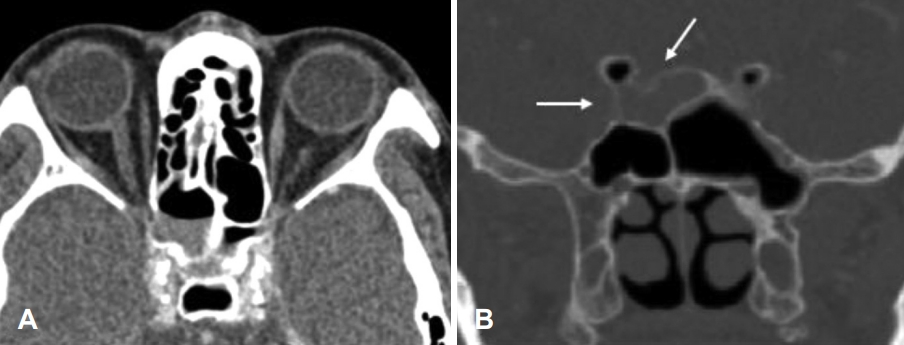
Fig.┬Ā4.Endoscopic view during operation. A: Chronic thickening of the mucous membrane around the opening of the Onodi cell. B: After removing the thick mucinous secretions inside the cells of Onodi, there were no defects in the inner optic canal or cranial base. 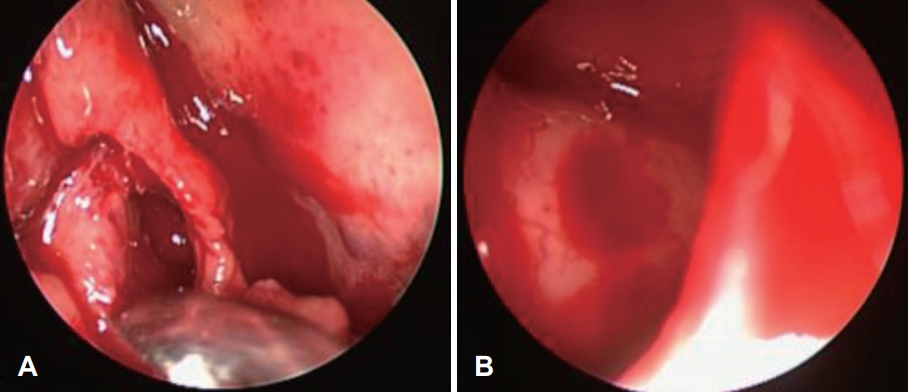
Fig.┬Ā5.Postoperative PNS CT. A and B: Postoperative axial (A) and coronal (B) contrast-enhanced imaging show no bony dehiscence with clear PNS, including clear Onodi cell, which was previously opacified with soft tissue density. C: Eyeball position at postoperative 2 months. Previously observed ptosis and exotropia have resolved and eye movements in all directions are normalized. PNS, paranasal sinus. 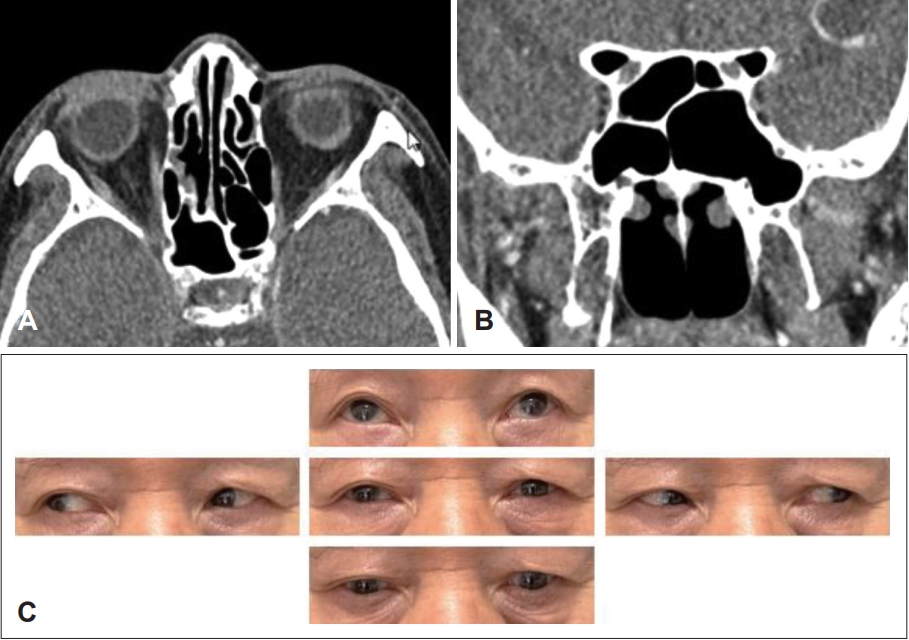
Fig.┬Ā6.Anatomical drawing of the cavernous-sinus region in a coronal section demonstrates the oculomotor nerve (III) is located just below the ACP (shown in green square), and the trochlear nerve (IV), ophthalmic nerve (V1), maxillary nerve (V2), and abducens nerve (VI) are more distantly located and inferiorly. ACP, anterior clinoid process. 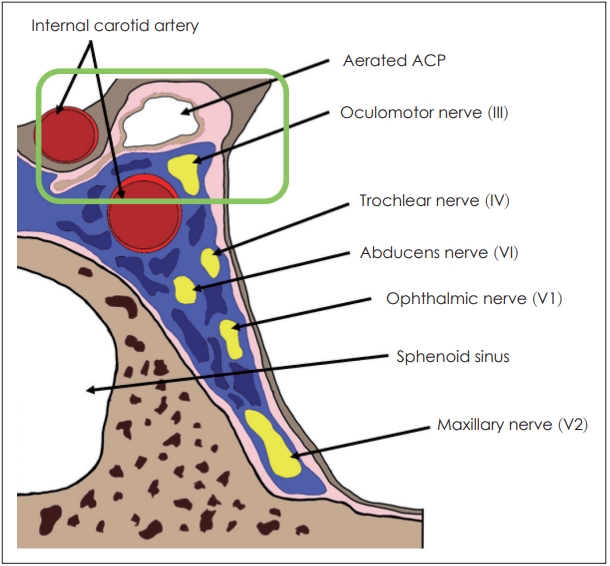
REFERENCES2. Sethi DS. Isolated sphenoid lesions: Diagnosis and management. Otolaryngol Head Neck Surg 1999;120(5):730-6.
3. Gilony D, Talmi YP, Bedrin L, Ben-Shosan Y, Kronenberg J. The clinical behavior of isolated sphenoid sinusitis. Otolaryngol Head Neck Surg 2007;136(4):610-5.
4. Huang EI, Kuo CL, Lee LW. A 16-year study on incidence and progression of diseased sphenoethmoidal (Onodi) cell. Biomed Res Int 2020;2020:2410415.
5. Fang C, Leavitt JA, Hodge DO, Holmes JM, Mohney BG, Chen JJ. Incidence and etiologies of acquired third nerve palsy using a population-based method. JAMA Ophthalmol 2017;135(1):23-8.
6. Kleid MS, Millar HS. Internal carotid artery epistaxis. Otolaryngol Head Neck Surg 1986;94(4):480-6.
7. Lee SJ, Kang YK, Lee ES, Kim JS. Prevalence of onodi cells in Korean based on computed tomography. Korean J Otorhinolaryngol-Head Neck Surg 2015;58(12):855-8.
8. Wang ZM, Kanoh N, Dai CF, Kutler DI, Xu R, Chi FL, et al. Isolated sphenoid sinus disease: An analysis of 122 cases. Ann Otol Rhinol Laryngol 2002;111(4):323-7.
9. Ruoppi P, Sepp├ż J, Pukkila M, Nuutinen J. Isolated sphenoid sinus diseases: Report of 39 cases. Arch Otolaryngol Head Neck Surg 2000;126(6):777-81.
10. Lawson W, Reino AJ. Isolated sphenoid sinus disease: An analysis of 132 cases. Laryngoscope 1997;107(12 Pt 1):1590-5.
11. El Mograbi A, Soudry E. Ocular cranial nerve palsies secondary to sphenoid sinusitis. World J Otorhinolaryngol Head Neck Surg 2017;3(1):49-53.
12. Hopf-Jensen S, Rubarth O, von D Ahe I, Riis P, Preuss H, Preiss M, et al. Isolated oculomotor nerve palsy caused by a mucocele of an aerated anterior clinoid process. Clin Neuroradiol 2014;24(2):161-4.
|
|
||||||||||||||||||||||||||||||||||||||||||||

 |
 |