 |
 |
AbstractBackground and ObjectivesPeritonsillar abscess (PTA) is an accumulation of pus between the palatine tonsil and pharyngeal constrictor muscle. It is a common cause of emergency on-call consultations among ENT doctors and occurs due to the possibility of sepsis, airway obstruction, and progression to deep neck infection. This study aims to compare the effectiveness of needle aspiration (NA) to incision & drainage (I&D) for the treatment of PTA.
Subjects and MethodFrom September 2018 to March 2020, 58 patients with PTA were admitted to our ENT Department. After a comprehensive diagnostic procedure, 38 patients were enrolled in the study and they underwent either I&D (20 patients) or NA (18 patients) treatment. Patients were discharged when edema decreased on the endoscopic findings and their symptoms improved, with a visual analogue scale (VAS) score <3 points. For each patient, we evaluated the abscess volume, age, body mass index, hypertension, diabetes mellitus, smoking and drinking history, abscess size, and duration of hospitalization. White blood cell (WBC) count, C-reactive protein (CRP) level, and erythrocyte sedimentation rate (ESR) were estimated on the 1st, 3rd, and 5th days of hospitalization.
IntroductionPeritonsillar abscess (PTA) is an accumulation of pus between the palatine tonsils and the pharyngeal constrictor muscles. It results from the progression of acute tonsillitis and has become a common cause of emergency on-call consultations among ENT doctors due to the possibility of sepsis, airway obstruction, and progression to deep neck infection [1,2].
The incidence rates of PTA vary across countries, from 9.7 per 100000 in Northern Ireland and 28.6 per 100000 in Sweden to 30.1 per 100000 in the United States [3-5]. The most common symptoms of PTA are sore throat, odynophagia, myalgia, and trismus [6].
Treatments of PTA include tonsillectomy, simple incision & drainage (I&D), and needle aspiration (NA) with antibiotics. In an American study, the distribution of PTA treatments was I&D in 54% of cases, NA in 32%, and tonsillectomy in 14% [3]. Previously, PTA had always been treated via quinsy tonsillectomy with antibiotics. However, due to the increased risk for postoperative bleeding and need for general anesthesia, I&D and NA have become first treatment choices in recent years [7,8]. While NA may be a first treatment choice due to its lower cost, ease to manipulation, and high success rate (96%), it’s important to also consider the potential for recurrence and the need for further treatment [3,9]. On the other hand, I&D has been associated with more efficient drainage of large amounts of pus and a reduction in the survival of anaerobic bacteria, which can contribute to the formation and persistence of abscesses by allowing air to circulate into the open spaces [9-11]. However, I&D is more painful, needs local anesthesia preoperatively, and requires hospitalization postoperatively. Therefore, there has been much debate on which method is better, with consideration of the risks and benefits [9-14].
In this study, we prospectively compared I&D to NA based on the pain score, volume of PTA, hospitalization duration, and blood test results in patients with PTA.
Subjects and MethodsParticipant selectionThis study was approved by Hospital Institutional Review Board (IRB No.: 2019-10-030-021), and all analyses adhered to the guidelines and regulations of our institution’s ethics committee. From September 2018 to March 2020, 58 patients with PTA were admitted to our ENT Department. All patients received a comprehensive diagnostic procedure, including history taking, physical examination, and radiologic imaging. Patients were randomly divided into two groups using a random number table method and received NA treatment and incision and drainage treatment respectively. PTA was drained using I&D or NA at the most pus-accumulated area based on CT. Two experienced ENT residents performed these procedures. Among 58 patients, 20 patients were excluded from the study due to young age (<19 years), procedure performed in another institution, early discharge (<3 days), and use of steroids due to underlying disease. Finally, 38 patients were enrolled in this study (I&D group, 20 patients vs. NA group, 18 patients) (Fig. 1). Patients were discharged when edema decreased on endoscopic findings and when their symptoms improved, with a VAS score <3 points.
Surgical and medical treatmentsI&DAfter local anesthesia using a lidocaine solution with epinephrine (2% lidocaine, epinephrine 1:100000; YUHAN, Seoul, South Korea), a 1-cm incision was performed with a No. 15 scalpel at the upper lateral side of the palatine tonsil between the fibrous capsule of the tonsil and the pharyngeal constrictor muscle. The incision was widened with mosquito forceps and purulent pus was drained (Fig. 2). The incision site was widened every morning and repeated until no pus came out.
NAA 10-cc syringe with a 22-G needle was inserted into the most protruding part of the upper tonsil, and then the pus was aspirated (Fig. 3).
CovariatesAge, body mass index (BMI), hypertension, diabetes mellitus, smoking and drinking history, abscess size, and duration of hospitalization were all evaluated. White blood cell (WBC) count, C-reactive protein (CRP) level, and erythrocyte sedimentation rate (ESR) were estimated on the 1st, 3rd, and 5th days of hospitalization. Pain scores using the visual analogue scale (VAS) were recorded every morning.
Statistical analysesComparisons of pre-treatment data (age, BMI, hypertension, diabetes, smoking, alcohol consumption, days hospitalized, abscess size, VAS score, WBC, ESR, CRP) between the two groups were analyzed using either the χ2-tests or the independent-sample t-tests. Repeated-measures analysis of variance for VAS, WBC, ESR, and CRP were also performed to analyze differences over time. SPSS version 26.0 for Windows (IBM Corp., Armonk, NY, USA) was used for statistical analyses, and a p-value <0.05 (two-sided) was considered statistically significant.
ResultsIn the I&D group, there were 12 males and 8 females with the mean age of 42.8±15.5 years. In the NA group, there were 13 males and 5 females with the mean age 40.3±14.7 years. There were no significant differences between groups in baseline characteristics, including age, BMI, hypertension, diabetes mellitus, smoking and drinking history, and abscess size. The duration of hospitalization was slightly longer in the NA group than in the I&D group (4.6±0.9 days vs. 5.3±1.2 days, p=0.051), but the difference was not statistically significant. In addition, the size of the abscess was bigger in the I&D group than in the NA group, but the difference was not statistically significant (6.4±3.9 cm3 vs. 4.8±7.2 cm3, p=0.380) (Table 1).
VAS scores on days 1 (initial), 2, 3, 4, and 5 of admission decreased each day after treatment but showed no statistical difference between groups. Similarly, the mean WBC count and mean CRP level gradually decreased each day in both groups without significant differences. The initial ESR level of the I&D group was significantly higher than that in the NA group (53.5±28.6 mm/h vs. 30.9±18.8 mm/h, p=0.022), and these levels decreased in both groups thereafter (Table 2).
DiscussionIn this study, there were no significant differences in the baseline characteristics between the I&D and NA groups, including underlying disease, abscess size, VAS score, WBC count, and CRP level, except for the initial ESR level. Postoperatively, there were no differences between groups in VAS score, WBC count, CRP level, and hospitalization duration.
PTA is one of the most common cervical infectious diseases in ENT field. If inadequately treated, it could progress to a deep neck infection that could cause upper airway obstruction and sepsis. Therefore, patients with PTA should be appropriately managed with medical treatment using antibiotics or surgical treatment, including quinsy tonsillectomy, I&D, or NA. In the past, there have been debates on which surgical treatment is better. Numerous reports stated that NA should be performed as a first treatment, since it is easy to perform and has comparable results with I&D [11,12,14-16]. Spires, et al. [12] investigated 62 patients with PTA who underwent NA (n=41) and I&D (n=21) but found no significant difference in the reformation of pus after the initial procedure between the NA (n=2) and I&D (n=0) groups. Moreover, they suggested that NA was easier to perform and can be done in the emergency room with limited instruments without risk. Similarly, Khokhar, et al. [11] reported that I&D or NA did not affect the treatment outcome of patients with PTA (35 in each group) after analyzing for odynophagia, fever, recurrence rate, and hospitalization days. Chi, et al. [14] also reported the treatment results of 110 patients with PTA (55 in each group), showing that the complication rate and length of hospital stay were similar between NA and I&D, but NA was superior to I&D based on the post-procedure pain score. On the other hand, some studies suggest that I&D is superior to NA due to the high failure rate of initial NA treatment [10,13,17]. Wolf, et al. [13] reviewed the medical records of 160 patients, with 86 in the NA group and 74 in the I&D group, showing that most patients of the NA group needed a repeat NA of up to 4 times and that the recurrence rate was higher compared to the I&D group. Mansour, et al. [17] performed a retrospective review of 182 patients, with 82 in the NA group and 100 in the I&D group, reporting a significantly lower length of hospital stay (2.42±0.99 days vs. 3±1.25 days) and lower risk of repeating the procedure in the I&D group than in the NA group. Additionally, a systematic review conducted in 2016 concluded that I&D may be associated with a lower chance of recurrence than NA [10]. There are also many studies comparing I&D and NA, but the results are varied with low reliability. Therefore, we performed a well-organized, prospective, randomized controlled study to compare I&D and NA.
The initial ESR was significantly higher in the I&D group compared to the NA group. However, there was little selection bias because patients were divided into two groups according to the order of hospital visit. There were no differences between the groups for other values except the initial ESR level, which means that I&D and NA did not differ in the prognosis and treatment outcomes.
Unlike NA, I&D requires local anesthesia prior to incision. I&D is known to be more fear-inducing, time-consuming, and mentally stressful than NA for both doctors and patients. However, NA showed similar treatment outcomes to I&D in this study. Therefore, it suggests that NA is an effective treatment for the initial treatment of PTA, which shows a recovery rate similar to that of I&D.
There are several advantages of this study. First, patients were randomly allocated according to the order of emergency department visit. Second, the volume of abscess in the initial CT were calculated by an independent professional radiologist to objectify our data. Third, this was a protocol-based, prospective, randomized controlled study, wherein the WBC, ESR, and CRP values were attained through planned laboratory examinations and subjective pain scores were assessed daily. Fourth, our hospital is the only hospital of its kind in our area. Therefore, there were no missed patients.
This study has several limitations. First, the number of enrolled patients was relatively small to get statistical significant. Before the pandemic, about 50 patients were admitted to treat PTA annually. However, after the spread of COVID-19, the number of patients abruptly decreased. When designing this study, we calculated a minimum sample size of at least 30 participants at each group to achieve statistical significance. However, only about 20 participants were enrolled at each group. Second, many recent studies have focused only on medical treatment using antibiotics without surgical treatment [18-20]. More research is needed on this point.
In conclusion, our study revealed no significant differences in hospital stay duration, VAS score, WBC counts or CRP level among patients admitted for PTA, whether they underwent I&D or NA. Favorable results were obtained in both groups without side effects. However, NA has an advantage over I & D in terms of ease of performance and the absence of the need for local anesthesia.
ACKNOWLEDGMENTSThis work was supported in part by a research grant (NRF-2019-R1G1A1-099842) from the National Research Foundation (NRF) of Korea.
NotesAuthor contributions Conceptualization: Young Ju Jin, Jin Lee. Data curation: Seung Yoon Han, Jeong Mi Lee. Formal analysis: Young Ju Jin, Jin Lee. Funding acquisition: Young Ju Jin. Investigation: Dong Hyun Kim, Jung-Hun Kwon, Hyung-Bon Koo. Methodology: Dong Hyun Kim, Jung-Hun Kwon, Hyung-Bon Koo. Project administration: Jin Lee. Hyung-Bon Koo. Resources: Se Jeong Jeon, Jeong Mi Lee. Software: Se Jeong Jeon. Supervision: Se Jeong Jeon, Jeong Mi Lee, Young Ju Jin. Validation: Young Ju Jin. Visualization: Seung Yoon Han, Young Ju Jin. Writing—original draft: Seung Yoon Han, Young Ju Jin. Writing—review & editing: Young Ju Jin, Jin Lee. Fig. 2.Incision & drainage was performed on a 24-year-old female patient. Peritonsillar swelling was observed using an endoscope. A: Left tonsil bulging was observed in the peritonsillar area (star). B: Peritonsillar abscess was detected in CT (star). After local anesthesia, a small incision was made at the location of the abscess (C) and the incision site was widened using mosquito forceps (D). 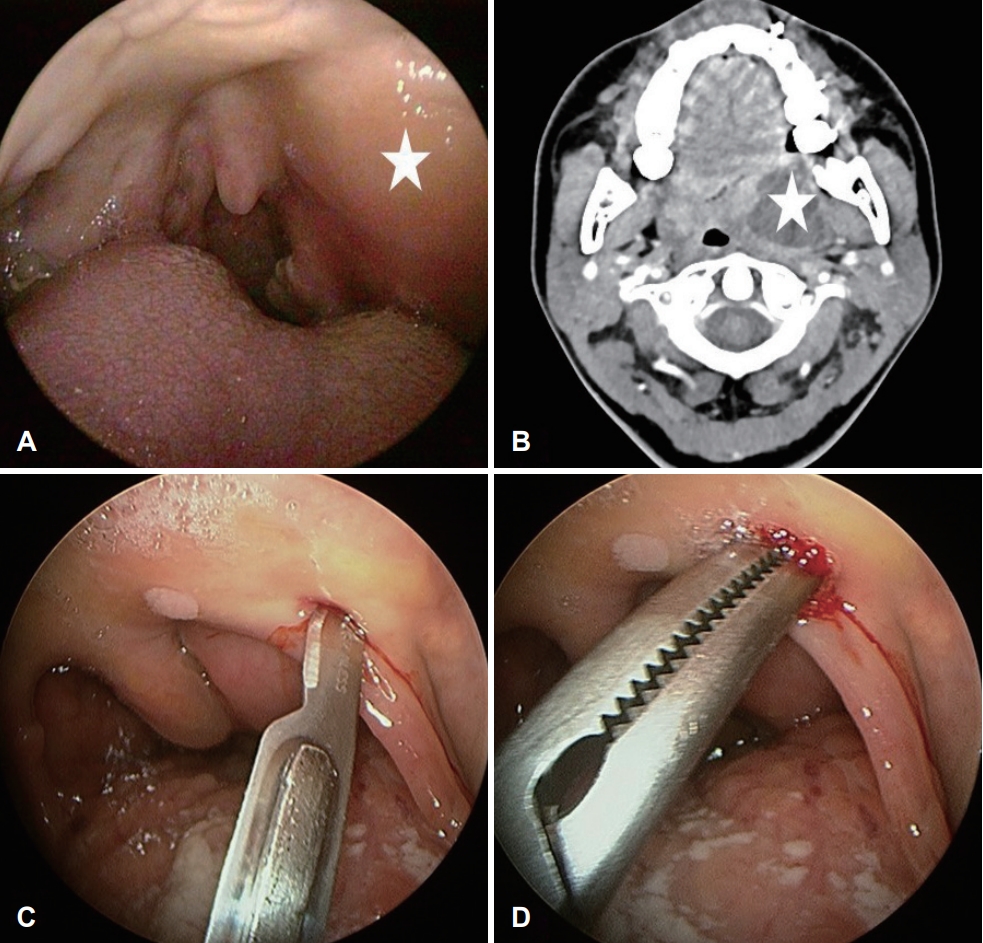
Fig. 3.Needle aspiration was performed on a 62-year-old male patient. Peritonsillar swelling was observed (A, asterisk) and the location of the abscess confirmed by CT (B, asterisk). A needle was inserted into the abscess (C) and pus was aspirated (D). 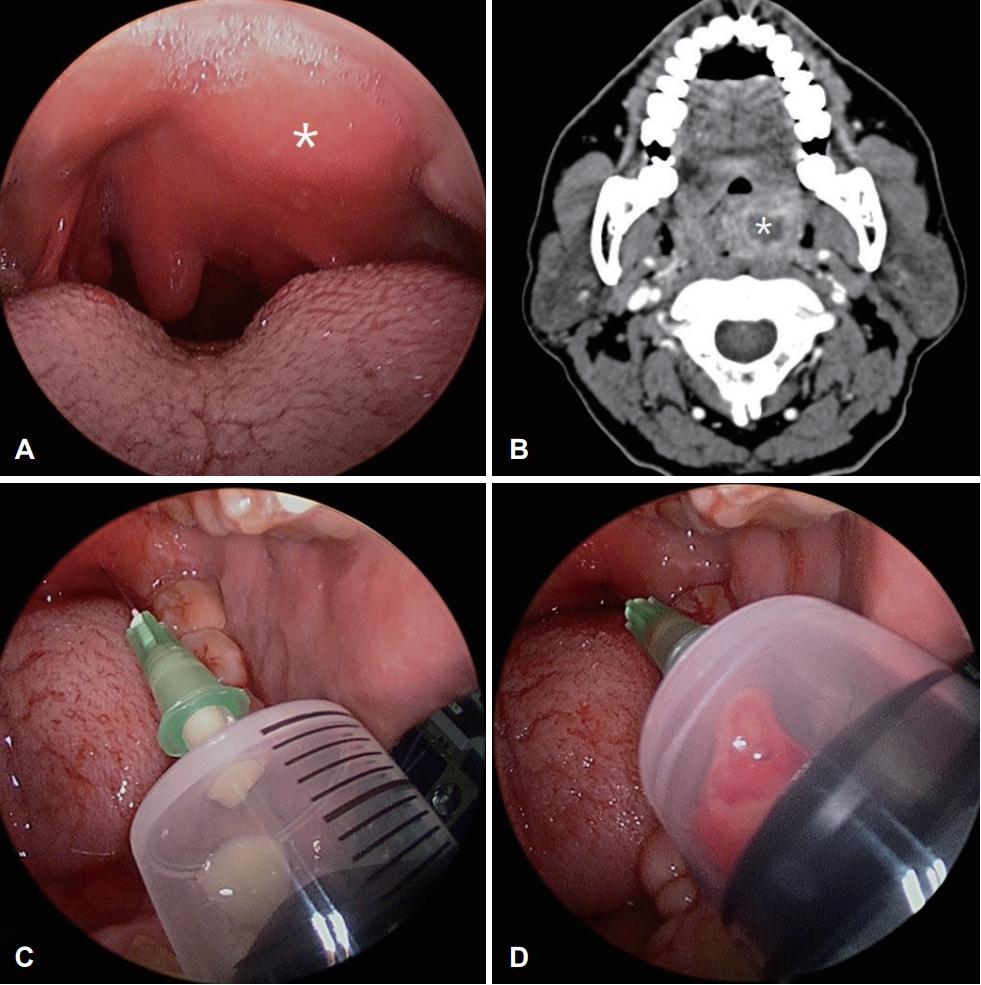
Table 1.General characteristics of participants Table 2.Initial clinical presentation, treatment response, and clinical outcome of two groups Data are presented as mean±standard deviation. Independent t-test or chi-square test, statistical significance at p<0.05. I&D, incision and drainage; NA, needle aspiration; HD, hospitalization day; WBC, white blood cell, CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; VAS, visual analogue scale REFERENCES1. Klug TE, Henriksen JJ, Fuursted K, Ovesen T. Significant pathogens in peritonsillar abscesses. Eur J Clin Microbiol Infect Dis 2011;30(5):619-27.
2. Bakir S, Tanriverdi MH, Gün R, Yorgancilar AE, Yildirim M, Tekbaş G, et al. Deep neck space infections: A retrospective review of 173 cases. Am J Otolaryngol 2012;33(1):56-63.
3. Herzon FS. Peritonsillar abscess: Incidence, current management practices, and a proposal for treatment guidelines. Laryngoscope 1995;105(S3):1-17.
4. Hanna BC, McMullan R, Gallagher G, Hedderwick S. The epidemiology of peritonsillar abscess disease in Northern Ireland. J Infect 2006;52(4):247-53.
5. Sunnergren O, Swanberg J, Mölstad S. Incidence, microbiology and clinical history of peritonsillar abscesses. Scand J Infect Dis 2008;40(9):752-5.
6. Lee JH, Park JG, Lee JD, Kim DW, Lee BD, Chang HS. A clinical analysis of peritonsillar abscess. J Clinical Otolaryngol 2003;14(2):282-7.
7. Giger R, Landis BN, Dulguerov P. Hemorrhage risk after quinsy tonsillectomy. Otolaryngol Head Neck Surg 2005;133(5):729-34.
8. Windfuhr JP, Chen YS. Immediate abscess tonsillectomy--a safe procedure? Auris Nasus Larynx 2001;28(4):323-7.
9. Windfuhr JP, Zurawski A. Peritonsillar abscess: Remember to always think twice. Eur Arch Otorhinolaryngol 2016;273(5):1269-81.
10. Chang BA, Thamboo A, Burton MJ, Diamond C, Nunez DA. Needle aspiration versus incision and drainage for the treatment of peritonsillar abscess. Cochrane Database Syst Rev 2016;12(12):CD006287.
11. Khokhar MR, Raza SN, Ayaz SB. Comparison of efficacy of needle aspiration versus incision and drainage in management of peritonsillar abscess. Pak Armed Forces Med J 2015;65(Suppl 2):S172-7.
12. Spires JR, Owens JJ, Woodson GE, Miller RH. Treatment of peritonsillar abscess. A prospective study of aspiration vs incision and drainage. Arch Otolaryngol Head Neck Surg 1987;113(9):984-6.
13. Wolf M, Even-Chen I, Kronenberg J. Peritonsillar abscess: Repeated needle aspiration versus incision and drainage. Ann Otol Rhinol Laryngol 1994;103(7):554-7.
14. Chi T, Yuan C, Tsao Y. Comparison of needle aspiration with incision and drainage for the treatment of peritonsillar abscess. WIMJ Open 2014;1(1):11-3.
16. Johnson RF, Stewart MG, Wright CC. An evidence-based review of the treatment of peritonsillar abscess. Otolaryngol Head Neck Surg 2003;128(3):332-43.
17. Mansour C, De Bonnecaze G, Mouchon E, Gallini A, Vergez S, Serrano E. Comparison of needle aspiration versus incision and drainage under local anaesthesia for the initial treatment of peritonsillar abscess. Eur Arch Otorhinolaryngol 2019;276(9):2595-601.
18. Forner D, Curry DE, Hancock K, MacKay C, Taylor SM, Corsten M, et al. Medical intervention alone vs surgical drainage for treatment of peritonsillar abscess: A systematic review and meta-analysis. Otolaryngol Head Neck Surg 2020;163(5):915-22.
|
|
||||||||||||||||||||||||||||||||||||||||

 |
 |