편도 및 아데노이드 절제술이 한국 소아의 음성에 미치는 영향
The Effect of Adenotonsillectomy on Korean Children’s Voice
Article information
Trans Abstract
Background and Objectives
Adenotonsillectomy is a commonly performed surgical procedure carried out by otolaryngologists for children. Anatomical changes to the vocal tract occur after the surgery and may alter the patient’s voice. This study evaluated the effects of adenotonsillectomy on the voice in Korean children.
Subjects and Method
A total of 20 children who underwent adenotonsillectomy were enrolled. The speech of patients was recorded before and at one month of the surgery and acoustic features, especially the formant frequency, were analyzed. Perceptual analysis was also carried out and the Pediatric Voice Handicap Index (PVHI) questionnaire was used to assess subjective changes in the children’s voice and the effects of these changes on social functions.
Results
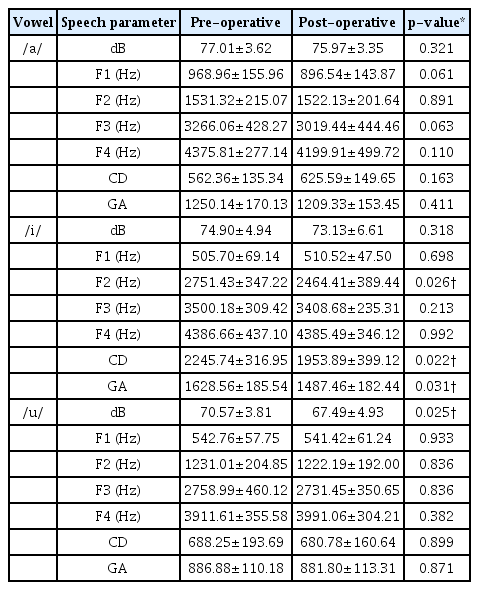
Acoustic analysis revealed significant decreases in the vowel /i/ in the second formant, compact-diffuse, and grave-acute features of the voice (p=0.026, 0.022, and 0.031, respectively). A significant decrease was also observed in the intensity of the voice for the vowel /u/ (p=0.025). Perceptual analysis revealed that 86.6% of patients’ voice recordings had postoperative changes. The mean preoperative PVHI score was 2.70±3.37, which decreased to 1.65±2.21 (p=0.011) after the surgery.
Conclusion
The results suggest that adenotonsillectomy affects Korean children’s voices both acoustically and perceptually.
Introduction
Adenotonsillectomy is the most commonly performed operation in children within the field of otorhinolaryngology [1]. Postoperative complications include bleeding, pain, and vocal changes, etc. Among them, changes to the voice after surgery often occur.
Fant [2] presented the source-filter theory in the acoustic theory of speech production. According to this theory, the human voice is produced through the larynx and vocal tract. The human vocal tract includes the oral, nasal, pharyngeal, and laryngeal cavities, which are important resonant cavities. Among them, the space within the oral and laryngeal cavities can be changed freely; thus, these cavities can create various resonance changes. Therefore, changes to the resonance properties after removal of the tonsils and adenoids located in the oral and nasal cavities may affect the voice. In children, in particular, the tonsils and adenoids occupy a relatively large area of the oral and nasal cavities and therefore have a large influence on the voice, because the vocal organs are in the process of growth and have yet to undergo voice mutation. Therefore, tonsillectomy or adenoidectomy, which changes the resonance energy in children, is important for childhood voice. Previous studies have produced conflicting results. Some have reported that the postoperative voice will be improved and others have reported that tonsillectomy has little effect on the voice, while others have reported that it can lead to velopharyngeal insufficiency [1,3-6]. These conflicting results may have resulted from the inclusion of different languages or a variety of methods for evaluating the voice. Therefore, our study explored vocal changes in a homogeneous population: Korean children who underwent adenotonsillectomy.
Subjects and Method
Patients
Our prospective study involved 20 pediatric patients with tonsillar (with or without adenoid) hypertrophy. One patient was diagnosed as having chronic tonsillitis with tonsillar hypertrophy. The study population included 13 boys and 7 girls, with a mean age of 7.6 years (Table 1). The inclusion criteria for this study were palatal tonsillar hypertrophy grade III or IV according to the scale suggested by Brodsky [7] and adenoid hypertrophy with 70% or more nasopharyngeal obstruction. Tonsillar hypertrophy was diagnosed by endoscopic direct observation and X-rays (lateral soft tissue neck view). Patients with a craniofacial or neurological syndrome and those with tonsillar tumors were excluded. We also excluded children who had definitive speech disturbances such as hoarseness, vocal paralysis, vocal fold polyps, laryngeal papilloma, airway infections, and children receiving speech therapy prior to surgery. Informed consent was obtained from all participants. This study was approved by the Institutional Review Board of Busan Saint Mary’s Hospital (approval no. BSM 2018-02).
Tonsillectomy and adenoidectomy
Tonsillectomy and bleeding control were performed using monopolar and bipolar cautery (Conmed Sabre 2400 Electrosurgical Unit; SOMA Technology Inc., Bloomfield, CT, USA) and adenoidectomy was performed using EVAC coblation (Coblator II Surgical System; ArthroCare Corp., Austin, TX, USA) via the transoral approach. All operations were performed by a single operator under general anesthesia.
Voice recordings (data collection)
Recordings were collected in a noise-controlled room on the day before surgery and at one month after surgery. Each subject was asked to phonate a Korean vowel, /a/, /i/, /u/, and four Korean sentences (이분은 아버지입니다/ibun-eun abeojiibnida/, 이것은 이발소입니다/igeos-eun ibalsoibnida/, 이것은 우체국입니다/igeos-eun uchegug-ibnida/, 우리 더불어서 책을 펴 봅시다/uli deobul-eoseo chaeg-eul pyeo bobsida/) at a comfortable volume. The voice was recorded at a sampling rate of 192 kHz and recording was performed using a voice recorder (ICD-SX 2000; Sony Co., Tokyo, Japan) with the patient placed at a distance of 20 cm from the microphone.
Acoustic analysis
The recorded voice was analyzed acoustically using the Praat software (ver. 5.2.16; University of Amsterdam, Amsterdam, the Netherlands). The number of decibels and the F1, F2, F3, and F4 formant frequencies of each vowel were measured. Other parameters of the vowel structure including the compact-diffuse (CD) and grave-acute (GA) features were also calculated from the formant frequency. The CD feature was obtained by subtracting F1 from F2. The GA feature was obtained by averaging the two values. According to the distinctive feature theory, the CD feature is regarded as an indicator of tongue elevation, while the GA feature is regarded as an indicator of tongue advancement [8]. Changes after surgery were evaluated by comparing the mean values of each parameter.
Perceptual analysis
Five otolaryngologists listened to and evaluated each patient’s voice before and at one month after adenotonsillectomy. Vowels and sentences were scored as 0 (no change), 1 (some change), and 2 (significant change) according to the degree of voice change after surgery (Table 2) [9].
Parental questionnaire
Before and at one month after surgery, caregivers were asked to complete a questionnaire to measure the subjective effects of voice disorders. The Pediatric Voice Handicap Index (PVHI) consists of 23 questions and is divided into functional, physical, and emotional sections containing 7, 9, and 7 questions, respectively. We used the Korean version that has been validated for Korean children [10]. Answers are scored from 0 to 4 (0: good, 4: very bad), and the minimum and maximum scores are 0 and 92, respectively.
Statistical analysis
For the acoustic analysis, the mean values of each pre- and postoperative parameter were compared using a paired t-test. For the perceptual analysis, overall agreement (OA) among the raters was calculated to determine the percentage of identical ratings between raters. The Fleiss kappa value (κ value) was also used to assess the inter-rater reliability of the five raters. Mean values of the pre- and postoperative PVHI scores were compared using the Wilcoxon signed-rank test. The SPSS Statistics ver. 25.0 statistical software package (IBM Corp., Armonk, NY, USA) was used for all statistical analyses. p values <0.05 were regarded as statistically significant.
Results
Acoustic analysis
In terms of the vowel /a/, the mean values of F1 and F3 had a relatively clear postoperative decrease (the preoperative F1 and F3 were 968.96±155.96 Hz and 3266.06±428.27 Hz, respectively, whereas the postoperative F1 and F3 were 896.54±143.87 Hz and 3019.44±444.46 Hz, respectively). However, the p value of F1 and F3 did not reach statistical significance (p=0.061 and 0.063, respectively) (Table 3). In terms of the vowel /i/, the mean values of F2 decreased significantly (the preoperative F2 was 2751.43±347.22 Hz and the postoperative F2 was 2464.41±389.44 Hz). CD and GA also decreased significantly (the preoperative CD and GA were 2245.74±316.95 and 1628.56±185.54, respectively, and the postoperative CD and GA were 1953.89±399.12 and 1487.46±182.44, respectively). No significant differences were identified in the remaining parameters (Table 3). In terms of the vowel /u/, the mean intensity differed significantly (the preoperative intensity was 70.57±3.81 dB and the postoperative intensity was 67.49± 4.93 dB). No significant changes were observed in the remaining parameters (Table 3).
Perceptual analysis
In terms of perceptual changes, 86.6% of cases were rated as ‘significant change’ and ‘some change.’ We classified these two groups together as ‘change.’ The κ value was -0.05 and the OA was 0.75 (Table 4).
Discussion
Resonance cavities include the oral cavity, nasal cavity, pharynx, and larynx. Among them, the space within the oral cavity and larynx can be freely transformed, leading to various vocal changes. Removal of the tonsils located on either side of the oral cavity and the adenoids located in the middle portion between the pharynx and nasal cavity causes a change in the resonance cavity after adenotonsillectomy and thus has a huge influence on the voice. This has been of great concern not only to occupational voice users but also to children who are still growing and to the general public.
Several studies have investigated vocal changes associated with tonsillectomy and adenoidectomy. Analysis of formant frequency is a helpful method that can predict changes in the upper airways that act as resonance organs. Previous research has found that variations in F1 reflect airway changes in apneic snorers, whereas variations in F2 reflect changes in the morphology of the tongue and variations in F3 reflect lip movements [11-13]. Some recent studies have used objective analysis of formants as well as subjective analyses. Some have reported that F0, F1, and F2 formant frequencies do not change significantly after tonsillectomy with or without adenoidectomy [14-17]. In contrast, Lin, et al. [18] observed an increase in F0 after surgery, and Kara, et al. [19] reported significant changes in F3 and F4 in 36 children at 3 months after adenotonsillectomy.
Our study revealed changes in acoustic characteristics of the voice after adenotonsillectomy. We observed a significant change in formant frequency was only for vowel /i/, which decreased significantly in F2, CD, and GA values. We believe that /i/ is most affected by postoperative tongue position changes because it is a front-high vowel. F2 is mainly dependent on the height of the tongue, CD is the parameter that reflects the height of the tongue, and GA is the parameter that determines the fore and aft position of the tongue. The oropharyngeal space after surgery becomes widened and causes the tongue to pronounce in the posteroinferior position. /u/ is a back-low vowel with no significant change in the movement of the tongue. /a/ is a back-high vowel with little fore and aft motion of the tongue. Therefore, these vowels appear not to change after surgery. The change in dB for the vowel /u/ was statistically significant, where the mean preoperative dB was 70.57±3.81 and the mean postoperative dB was 67.49±4.93 (p=0.025). However, a 3-dB change may not be large enough to be of clinical significance because sound is perceived to be twice as loud for every increase of 10 dB.
Our results differ slightly from those of previous studies, due to the nature of research measuring vocal parameters. The measurement of vocal parameters is highly sensitive, so statistical values vary depending on the selection of subjects and the postoperative follow-up duration.
The degree of tonsillar hypertrophy varies from grade I to grade IV, depending on size. Saida and Hirose [14] reported that vocal changes occur when grade III or higher tonsils are removed. Ilk, et al. [17] reported that the greater the grade of tonsil, the more severe the change of postoperative voice. Therefore, we included patients with grade III or IV tonsillar hypertrophy. We also limited the age range of subjects, because children under the age of 5 years may not be able to phonate as requested, and children aged 10 years and older may have already experienced voice mutation.
In vocal analysis, perceptual analysis of subjective vocal changes is important. Previous perceptual analyses performed by language pathologists or otolaryngologists have yielded variable results. Chuma, et al. [15] reported that the majority of perceptual categories did not change significantly postoperatively, except for a significant decrease in hyponasality. Lunderborg, et al. [20] reported that their study population had more hyponasality, compressed/throaty voice, and lower pitch, and that these were significantly improved and normalized after surgery. In our study, we found that most patients had postoperative changes, indicating the possibility of vocal change after surgery. Although the κ value was low, the OA was 0.75, which was highly consistent among raters. However, a particular limitation of our study is that we did not investigate detailed perceptual parameters such as hoarseness, breathiness, nasality, pitch, roughness, etc., and we did not aim to reach a consensus about the definition of ‘voice change.’
We used the PVHI to conduct a subjective analysis according to the parents’ response. The PVHI is a validated questionnaire for assessing the psychosocial aspects of voice disorders. Naraghi, et al. [21] recruited 86 children aged 3-13 years and reported an improved PVHI score after tonsillectomy with or without adenoidectomy (mean preoperative score: 14.39, mean postoperative score: 2.93). A study that compared the PVHI scores of normal and dysphonic groups of Korean children aged 3-11 years reported a score of 2.33 for the control group (mean age: 7.73±1.43 years, n=15) and 23.13 for a dysphonia group (mean age: 7.33±2.87 years, n=15) diagnosed with vocal cord nodules [22]. In our study, the mean preoperative score was 2.70±3.37 and the mean postoperative score was 1.65±2.21 (p=0.011). Although the difference before and after surgery was statistically significant, the preoperative PVHI scores of our patients were very similar to those of normal Korean children, and the postoperative PVHI scores were within the normal range. This could not explained may be a placebo effect related to the parents’ expectations of a positive change postoperatively. Therefore, this result indicates that, at the least, the parents did not perceive a negative change in their child’s voice after surgery.
In conclusion, tonsillectomy with or without adenoidectomy may affect the voice acoustically and perceptually in Korean children. Voice research is highly sensitive, so our study of postoperative vocal changes in Korean children is valuable. When performing adenotonsillectomy, consideration should be given to the possibility that Korean children’s voices may be altered after surgery. In the future, it will be necessary to study more diverse subject groups, use various research methods, and allow a longer follow-up duration for Korean children who undergo adenotonsillectomy.