설소대 단축증 환아에서 언어발달과 행동-정서적 문제와의 상관관계 분석
Association Between the Language Development and Behavioral-Emotional Problems in Children With Ankyloglossia
Article information
Trans Abstract
Background and Objectives
The study attempted to clarify the correlation between the degree of behavioral-emotional problems and language development in patients with ankyloglossia and to identify pre- and post-operative changes in pronunciation, language, and behavioral- emotional problems.
Subjects and Method
This prospective cohort study was conducted at a tertiary academic center. Patients with ankyloglossia exhibiting articulation disorders were divided into normal and language delay groups according to the degree of language development. Articulation was evaluated using the Korean-specific Urimal Test of Articulation and Phonation (U-TAP), and language development was evaluated using the Preschool Receptive-Expressive Language Scale (PRES). The difference in the degree of behavioral-emotional development between the two groups was analyzed using the Strengths and Difficulties Questionnaire test. Moreover, changes in articulation, language development, and behavioral-emotional development scores were compared before and 3 months post-operatively in the two groups.
Results
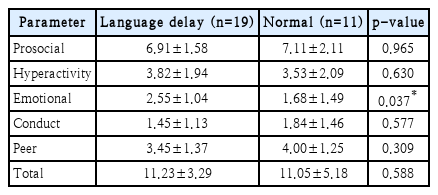
Thirty patients with ankyloglossia were enrolled and classified into the normal group (n=11) and language delay group (n=19). Children of the language delay group exhibited significantly delayed improvements in emotional symptoms compared to those in the normal group (2.55±1.04 vs. 1.68±1.49 in language delay vs. normal group, respectively; p=0.037). The UTAP and PRES test scores were improved three months post-operatively in the entire group, but there was no significant difference after surgery when compared between the two groups.
Conclusion
Behavioral-emotional development was delayed in patients with ankyloglossia accompanied by language delay. Furthermore, articulation and language development improved three months after frenoplasty in all patients. However, behavioral-emotional development was delayed in patients with ankyloglossia accompanied by language delay.
Introduction
Ankyloglossia or tongue-tie is a congenital variation resulting in a short lingual frenulum, which can cause restricted tongue movement and the function of tongue as well [1]. Various studies have shown that such restrictions on tongue movement can lead to breastfeeding and language development problems, and poor oral hygiene and social adaptation [2,3]. Additionally, many studies show that delays in language development in children affect social development [4]. Socio-emotional and behavioral developments are closely related to receptive and expressive languages, which indicates that screening both development types is necessary for toddlers with potential language delays [4,5].
Although language delay can be observed in patients with ankyloglossia, no study has investigated whether behavioral or emotional problems and language delay in patients with ankyloglossia are related to each other [6].
In this study, we compared and analyzed the differences in behavioral-emotional problems according to the degree of language development in patients with ankyloglossia and how they can affect patients by comparing articulation, language development, and behavior/emotional development before and after surgery.
Subjects and Methods
Subjects and study design
Forty-four consecutive patients who were treated by our clinic for a short frenulum between May 2018 and February 2020 were enrolled. The inclusion criteria were 1) patients aged ≥3 years and 2) those with Ankyloglossia greater than Classification 1 based on the Kotlow assessment tool [7]. Analysis of sex, age, allergy, breastfeeding problems and birth history was conducted to evaluate the baseline of patient characteristics.
The exclusion criteria were: 1) ankyloglossia without having undergone the articulation test prior to surgery, and 2) loss at 3 months follow-up or not having undergone the test after surgery. Informed consent was obtained according to the Declaration of Helsinki, and the study protocol was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong (IRB number 2016-06-008).
Assessment methods and questionnaires
The subjects were evaluated for articulation, language development, and behavioral-emotional development. Articulation was evaluated by an experienced speech-language pathologist (SLP) using the Korean-specific Urimal Test of Articulation and Phonation (U-TAP). Language development was performed by the SLP using the Preschool Receptive-Expressive Language Scale (PRES). Behavioral-emotional development evaluation was performed using the Strengths and Difficulties Questionnaire (SDQ-Kr). The self-reported Korean version of the SDQ (SDQ-Kr) is a reliable and valid screening instrument for assessing emotional and behavioral symptoms in Korean children [8]. SLP performed pre- and postoperative articulation tests without knowing any information of the operation.
U-TAP is an articulation and phonation test that is targeted for children in pre- school age. It evaluates articulation and phonation at the sentence and word levels by examining consonants and vowels. The results show whether the articulation development is normal through calculating children’s articulation errors [9].
PRES is the most frequently performed test in Korea to evaluate language development for children in pre-school age, which measures receptive language age and expressive language age through investigating different aspects of performance in language [10].
The SDQ-Kr examines 25 statements regarding child’s behavior over the past six months. The informant is needed to answer whether it is “Not true,” “Partially true,” or “Certainly true” for each statement. The middle option is assigned a value of 1 when calculating the score and the remaining two options are assigned values of 0 or 2, depending on each statement. Five scores ranging from 0 to 10 can be calculated based on the answers to the five questions. Four of these scores are summed to obtain a total difficulty score. Conversely, the fifth—the prosocial score—reflects social strength [11].
Surgical procedure
We performed a simple frenotomy or 4-Flap Z-frenuloplasty under general anesthesia. In previous our study, there was no significant differences in the improvement rate in the articulation test results between the two procedures [12]. Thus, we selected procedures considering tongue-tie classification and patient preference. Surgical procedure was referred from our study presented above.
In simple frenotomy, a mouth gag was used to keep the mouth open. A 2-0 silk suture was placed at the tip of the tongue and was used to retract the tongue superiorly to expose the frenulum. The frenulum was aligned with the midline after injecting 1:200000 lidocaine with epinephrine. The frenulum was divided using the Bovie electro-surgical instruments. Adequate dissection of the mucosal layer of the tongue base was carried out to secure a sufficient length of the frenulum. After the release of the frenulum, the tongue mucosa was closed with a resorbable suture (Fig. 1).
In 4-Flap Z-frenuloplasty, the tongue tip was elevated in the same way as in the simple frenotomy. Ink markings were made as shown in the following image (Fig. 2). Subsequently, 1:200000 lidocaine with epinephrine was injected, and a number 15 blade was used to incise the markings. Iris scissors were used to mobilize the flaps of slightly greater thickness to include some glandular tissue at the base of the flaps. The flaps were transposed from an “ABCD” order to a “CADB” order. Finally, the transposed flaps were sutured with interrupted 4-0 vicryl sutures.
Statistical analysis
Statistical analyses were performed using the R software package (http://www.r-project.org).
Demographic differences between the two groups were assessed using two-sided Fisher’s exact test to compare continuous and categorical variables. The comparison of social development between the two groups was assessed using the Wilcoxon rank-sum test. The Wilcoxon signed-rank test was used to compare the pre- and post-operative test scores. Statistical significance was set at p<0.05.
Results
The patient selection, classification, and application of each test are shown in Fig. 3. First, forty-four children with ankyloglossia were enrolled, and we wanted to perform U-TAP test in all patients. However, two of them did not cooperate, and six were not tested because their parents did not want to perform examination. Thus, 36 patients underwent the U-TAP test. Only two patients were normal, and 34 exhibited problems with articulation by >1 standard deviation (SD) in the U-TAP test. Most patients showed articulation problems, which we could not classify using the U-TAP test.

Study flowchart. Std, standard deviation; U-TAP, Koreanspecific Urimal Test of Articulation and Phonation; PRES, Preschool Receptive-Expressive Language Scale; SDQ-Kr; Strengths and Difficulties Questionnaire; f/u, follow up.
Thus, we additionally performed the PRES test in 30 patients who were able to cooperate. Six patients who did not want to undergo further examination were excluded in this process. We defined patients whose developmental age was <1 year below their living age as patients with language delay. Thirty patients were classified into the normal (n=11) and language delay (n=19) groups. No significant differences existed in terms of their demographics, including age, body mass index, or sex, between the two groups (Table 1). In addition, no significant differences were found in disease, medication, term, allergy, or breastfeeding history between the two groups. In these 30 patients, U-TAP test was performed. Only one patient was normal (normal group;1, language delay group;0), and 4 patients exhibited problems with articulation by >1 SD (normal group;2, language delay group;2), and 25 patients exhibited problems with articulation by >2SD (normal group;8, language delay group;17).
Thirty patients also underwent the SDQ-Kr test. A significant difference was found in emotional symptoms (2.55±1.04 vs. 1.68±1.49 in language delay vs. normal group, respectively; p=0.037) (Table 2). However, no significant differences were found between the two groups in terms of social behavior, hyperactivity, behavioral problems, or peer problems.
Frenoplasty or Z-frenuloplasty was performed in all patients. Three months after the surgery, follow-up U-TAP, PRES, and SDQ-Kr tests were performed. Postoperatively, patient participation decreased (U-TAP in 17 patients, PRES in 13, and SDQ-Kr test in 10). A total of 10 patients underwent all three tests after surgery.
Table 3 shows the changes in the U-TAP, PRES, and SDQ-Kr test results before and after surgery in patients who completed these three tests at 3 months after surgery. The U-TAP scores significantly improved after surgery in the entire group (72.79±6.7 vs. 82.55±9.4 pre-op vs. post-op, respectively; p=0.009). PRES scores also significantly improved after surgery in the entire group (30.6±6.2 vs. 38.4±9.7 pre-op vs. post-op respectively; p=0.006). However, there was no significant difference after surgery when divided into the normal (n=5) and language delay groups (n=5). Moreover, there was no significant change in the SDQ-Kr test results before and after surgery in all patients. There were no statistically significant differences between the pre- and post-operative score changes for each sub-item of the SDQ-Kr (Table 4).

Comparison of pre- and post-frenoplasty U-TAP, PRES, and SDQ-Kr test results between the language delay and normal groups who completed these three tests at 3 months after surgery
Discussion
The prevalence of ankyloglossia reportedly varies widely. This may explain the existence of the various diagnostic criteria. Many studies have assessed the structural problems that can occur in children with ankyloglossia [13-15]. Due to the movement restriction of the tongue tip, articulation problems are mainly encountered in the pronunciation of consonants, such as s, z, t, d, r, l, j, ch, and th. Children with articulation problems may experience social and emotional problems. Many studies have shown that language delays can be a social and emotional problem. Early language delay may have influenced the development of emotions, particularly emotional self-regulation. Delayed language also weakens the parent-child bond, indicating that reduced language may interfere with the establishment of close attachment bonds [16,17]. However, few studies have assessed how the delay in language development caused by ankyloglossia affects the behavioralemotional development of children.
In this study, we classified patients with ankyloglossia into two groups according to their level of language development by comparing the degree of behavioral-emotional problems through PRES and SDQ-Kr test scores. A significant developmental delay was observed in emotional symptoms when language development was delayed. This satisfied the study hypothesis that limited tongue movement due to ankyloglossia can cause delays in language development, and that this delay can further cause delays in behavioral-emotional development. This suggests that a more active intervention may need to be considered for patients with ankyloglossia showing delayed language development.
However, on analyzing the score change of each item in the SDQ-Kr before and after surgery, behavioral-emotional development was not achieved after surgery. There are two main explanations for the results. First, in the case of behavioralemotional development problems, recovery may take longer than in the case of articulation or language development problems. Second, if normal development is not achieved due to language development delay during the social development stage in children, behavioral-emotional development may not be achieved even if language development is restored. If behavioral-emotional recovery is not achieved, early surgical correction may be required before a delay in social development occurs, when language development delay is found in a child with ankyloglossia.
Therefore, whether the development of sociality occurs is necessary to confirm in future long-term studies. This can be an important basis for determining the treatment method and timing when language development delay is confirmed in children with ankyloglossia.
This study had several limitations. The first limitation was the short study period. Because follow-up was performed only up to three months after surgery, a long-term study is needed. Second, our sample size was small. Further studies with larger sample sizes are required. Third, in patients receiving speech therapy, it is difficult to determine whether improvement in articulation and speech development was achieved only through surgical treatment.
Nevertheless, to our knowledge, this is the first study to clarify the correlation between the degree of behavioral-emotional problems and language development in patients with ankyloglossia. We found that patients with ankyloglossia showing language delay suffered more emotional problems than did those with normal language development. Further studies in larger cohorts will help to confirm the association between language development and other behavioral-emotional problems in patients with ankyloglossia.
In conclusion, based on the degree of language development, patients with ankyloglossia were divided into normal and language delay groups. The degree of social development was compared between the two groups, and the language delay group exhibited significantly lower scores in the emotional category than did the normal group. Moreover, in the comparison between the pre- and post-operative levels, articulation and language development improved three months after frenoplasty in overall patients. However, behavioral-emotional development was delayed in the case of patients with ankyloglossia accompanied by language delay.
Acknowledgements
None
Notes
Author Contribution
Conceptualization: Jong Hwan Lee, Su Il Kim, Young Chan Lee. Data curation: Jong Hwan Lee. Formal analysis: Tae Hoon Kim. Investigation: Seul Ah Lee, Tae Hoon Kim. Methodology: Jong Hwan Lee, Su Il Kim. Software: Jong Hwan Lee, Su Il Kim. Supervision: Young Chan Lee, Young-Gyu Eun. Visualization: Jong Hwan Lee. Writing—original draft: Jong Hwan Lee, Su Il Kim, Young Chan Lee. Writing—review & editing: Jong Hwan Lee, Su Il Kim.