외이도 종물로 나타난 전정신경초종: 새로운 2예 보고와 문헌 고찰
Extended Vestibular Schwannoma Presenting as an External Auditory Canal Mass: Two New Cases and Review of the Literature
Article information
Trans Abstract
This article describes two rare cases of vestibular schwannoma extending to the external auditory canal (EAC). Vestibular schwannomas typically arise from the internal acoustic canal and have a slow growth rate, rarely extending to the middle ear extension and even rarer EAC. The article highlights the importance of considering vestibular schwannoma as a differential diagnosis in patients with masses in the EAC and the need for early diagnosis and treatment to prevent potential complications.
Introduction
Vestibular schwannomas (VS) are benign tumors that frequently occur at the cerebellopontine angle (CPA), usually arising from the internal acoustic canal (IAC). Intralabyrinthine schwannomas, on the other hand, are far less common (1% of all VS) and they tend to extend toward the CPA due to the absence of a bony barrier [1]. And VS have a slow growth rate, as previously reported in the literature, with overall mean growth rates ranging from 1.15 to 2.4 mm/year [2]. So the lateral extension of a VS involving the middle ear is very rarely reported. Furthermore, it is even more rarely to be found in the form of an external auditory canal (EAC) mass and only a few cases have been reported in the literature to date. To the best of our knowledge, only five cases have been reported from 1950 to 2021. Here, we present two cases of VS presenting as tumor of the EAC.
Case
Case 1
A 44-year-old female presented to our hospital with right EAC mass. She experienced sudden deafness 10 years ago, and since then, her right ear has been deaf. Initial otoscopic examination revealed bulging of the right tympanic membrane and a multinodular mass with a soft, gelatinous consistency in front of it (Fig. 1). Pure-tone audiometry showed that her right ear was deaf, whereas her left ear was normal.
Result of otoscopic examination of case 1 showing a multinodular mass with a soft, gelatinous consistency in front of the tympanic membrane.
The contrast enhanced CT scan identified an IAC enlargement and the presence of homogeneous mass in lower portion of the middle ear near the round window extending to the EAC. This iso-dense mass was also continued with the soft tissue density of cochlea space through the round window (Fig. 2). MRI was performed for detailed differentiation of the middle ear mass. It showed a large mass in the CPA and IAC extending to the cochlea and vestibule. The mass was hypointense and enhanced in the T2- and T1-weighted images, respectively (Fig. 3). The imaging finding indicated that the tumor was consistent with multiple schwannomas involving the right CPA, vestibule, semicircular canal, and right middle ear cavity. Surgical resection was planned using the transotic approach to properly expose the tumor.
Right side internal acoustic canal enlargement when compared with the contralateral side (A) and the presence of homogeneous mass in lower portion of the right middle ear near the round window extending to the external auditory canal (B) on enhanced axial CT scan of case 1.
MR findings of case 1. T2-weighted image (A) showing a mass that is isointense to the adjacent brain, located in the cerebellopontine angle and internal acoustic canal, and extending to the cochlea and vestibule. The mass is enhanced in the T1-weighted image (B).
During the operation, the tumor filling the mesotympanum and hypotympanum was confirmed and removed. It was estimated that the tumor extended to the middle ear through the round window. It was also found that the semicircular canal, common crus, inside of the vestibule, and IAC were all filled with tumors, which were all removed. In addition, the neurosurgeon removed the tumors at the CPA and attempted to dissect the brainstem, facial nerve, and tumor; however, some tumors were left due to severe adhesion. For these remaining tumors, Gamma Knife surgery was planned to be performed later. The pathologic finding indicated schwannoma.
After surgery, the patient developed House-Brackmann grade 3 right facial paralysis. Furthermore, the patient developed cerebrospinal fluid (CSF) otorrhea about 2 weeks following surgery, and surgical repair of the dura defect was successfully performed. After confirming the complete cessation of the CSF otorrhea, Gamma Knife surgery was also performed for the remaining tumor near the brainstem. About 1 year after surgery, the patient recovered to House-Brackmann grade 1 for the right facial paralysis. The patient was followed up for 3 years, and no tumor recurrence or late complications were noted.
Case 2
A 62-year-old male underwent brain MRI due to hemifacial spasm. This led to the detection of enhancing mass in the left IAC. Thus, he was referred for further evaluation (Fig. 4). He had left tinnitus and hearing impairment 10 years ago but did not receive any treatment. Otoscopic examination revealed a bulging mass inside the tympanic membrane; thus, an incisional biopsy was performed. The result of the histological examination indicated schwannoma. Gamma Knife surgery was performed to control the mass. After 2 years, the patient revisited our hospital due to complaints of left otorrhea, and otoscopic examination revealed mass in the EAC (Fig. 5). Brain MRI showed that the previously identified lesion progressed and extended to the middle ear and EAC (Fig. 4). Surgical treatment using the translabyrinthine approach was considered for the schwannoma extending to the IAC, middle ear, and EAC; however, the patient was lost to follow-up.
Initial MRI of case 2: hypointensity in the T2-weighted image (A), mass from the cerebellopontine angle to the internal acoustic canal enhanced in the T1-weighted image (B). Follow-up MRI of case 2: hypointensity in the T2-weighted image (C) and enhancement in the T1-weighted image (D), extending to the middle ear and external auditory canal.
Discussion
Vestibular schwannoma is a benign tumor, and in 80% of VS, it is found as a CPA tumor. It commonly occurs on the Schwann cell of the vestibular nerve sheath within the IAC and tends to extend to the CPA due to the absence of bony barrier. Intralabyrinthine schwannomas are much less common (1% of all VS), with a prevalence of 0.1%-0.4%; they occur in the peripheral intralabyrinthine branches of the vestibulocochlear nerve [3]. Tieleman, et al. [4] suggested that most of the inner ear schwannomas (80%) occur in the cochlea, particularly in the basal and second turn of the cochlea and more frequently in the scala tympani.
In a literature review, there were a few cases where VS has progressed and invaded the middle ear, but cases where it has invaded the EAC and diagnosed as EAC mass were very rare that only five cases have been reported since the first report by Trans, et al. in 1987 (Table 1) [5-9]. In these cases, it is difficult to accurately identify the origin of the tumor, and the tumor that originated in the IAC, where VS commonly occurs, can be considered to have progressed medially to the CPA and externally to the inner and middle ears. Alternatively, it is conceivable that the tumor that occurred within the labyrinth progressed medially to the IAC and CPA and externally to the middle ear. Intralabyrinthine schwannoma is a tumor originating from the cochlea, vestibule, or semicircular canals corresponding to the membranous labyrinth. Primary labyrinthine schwannoma was previously considered rare, but more than 150 cases have already been reported until recently [10]. In addition, case of multifocal origin tumors independently from the IAC and intralabyrinthine can be considered. However, multiple unilateral VS occurring without the features of neurofibromatosis type 2 are considered very rare as only three cases have been reported to date [11].
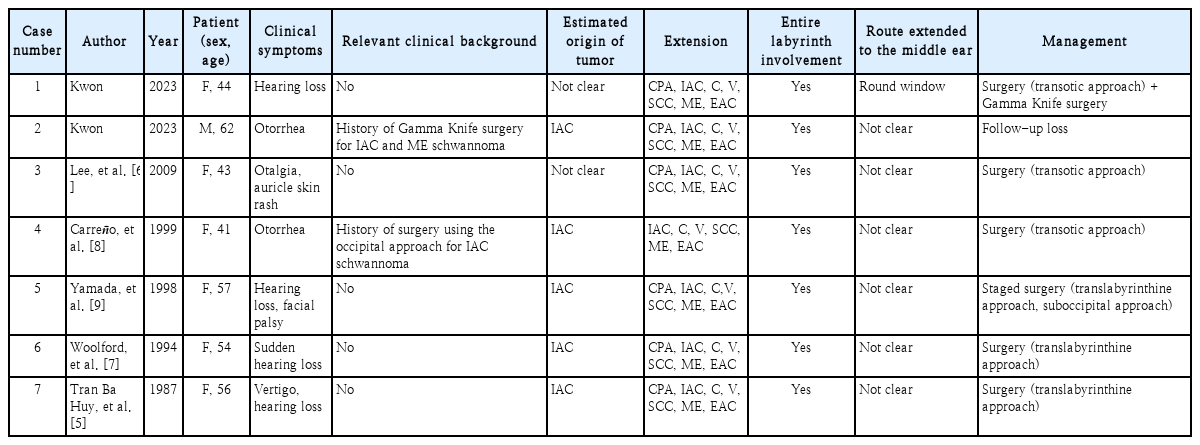
Clinical characteristics of patients (two presented in this article and five reported in the literature) with VS extending to the EAC
Regarding the case where VS has progressed to the EAC at the time of diagnosis, none of the studies clearly mentioned the origin of the tumor. Furthermore, in all these studies, the tumors have been removed through surgical treatment using the translabyrinthine approach. The patients presented here were middle-aged (43-57 years old) individuals, and the second patient is the first reported male case. Both of them did not have relevant clinical backgrounds, such as neurofibromatosis.
The difference between our first case and the other reported cases is that in the former, the tumor progressed into the middle ear through a round window, based on the CT and surgical findings, which is consistent with Venkatasamy, et al.’s [1] claims regarding the progression of the VS. In most cases of EAC mass, the first selected imaging test would be probably contrast enhanced temporal bone CT scan. The axial view shown in this case showed connectivity of mass through the round window and enlargement of IAC which is not frequent findings in an EAC mass. This suggests that when the EAC mass invades the middle ear, careful examination of the round window and confirmation of IAC enlargement can provide useful information for early differential diagnosis of extensive VS.
Vestibular schwannoma has a very slow growth rate, and there are different views regarding aggressive treatment of the tumor at the time of diagnosis. Our second case and the case reported by Carreño, et al. [8] had tumor recurrence after the initial treatment. Careful preoperative assessment of the tumor extension and selection of appropriate treatment are mandatory for extended VS.
Through further analysis and consideration of VS extending to the middle ear and EAC, which is rare, as in the present cases, it will be possible to determine the cases requiring early aggressive treatment. And since round window seems to be the main route of extension of VS to the middle ear, careful examination of theround window on MRI is mandatory before surgical treatment.
Acknowledgements
This work was supported by Biomedical Research Institute grant, Kyungpook National University Hospital (2017).
Notes
Author contributions
Conceptualization: Myung Hoon Yoo. Data curation: Ki-Su Park, Kyu-Yup Lee, Myung Hoon Yoo. Formal analysis: Ha Gyung Kwon, Myung Hoon Yoo. Funding acquisition: Kyu-Yup Lee, Myung Hoon Yoo. Supervision: Ki-Su Park, Myung Hoon Yoo. Validation: Ki-Su Park, Myung Hoon Yoo. Writing—original draft: Ha Gyung Kwon. Writing—review & editing: Ki-Su Park, Kyu-Yup Lee, Myung Hoon Yoo.