고막외이도피판 거상 없이 시행하는 내시경적 밀어넣기 연골막 고막성형술의 효과에 대한 연구
Efficacy of Endoscopic Push-Through Perichondrial Myringoplasty Without Tympanomeatal Flap Elevation
Article information
Trans Abstract
Background and Objectives
Endoscopic ear surgery has gained widespread application in otology as a minimally invasive surgical technique that minimizes patient morbidity. This study aimed to evaluate the surgical and audiological outcomes of endoscopic push-through perichondrial myringoplasty (EPPM) without tympanomeatal flap elevation.
Subjects and Method
We retrospectively reviewed the medical records of 34 patients with chronic otitis media who underwent EPPM without tympanomeatal flap elevation between July 2018 and January 2023. The primary outcomes, including graft success rate, audiological outcomes, and surgical complications, were evaluated.
Results
Among the 34 patients, 22 were female and 12 were male. The mean age was 58.0±16.1 (18-83) years and the mean follow-up period was 15.7±10.4 (4-45) months. The overall graft success rate was 91.2% (31/34). The mean preoperative and postoperative air-bone gaps (ABG) were 15.5±11.6 dB and 6.9±6.7 dB, respectively. The mean postoperative ABG significantly improved compared to the mean preoperative ABG (p<0.001). A postoperative ABG ≤20 dB, indicating successful hearing outcomes, was achieved in 92.3% (24/26) of the patients. No major intra- or postoperative complications were observed.
Conclusion
This study revealed that EPPM without tympanomeatal flap elevation is an effective surgical technique and that it provided favorable surgical and audiological outcomes in patients with chronic otitis media.
Introduction
Perforation of the tympanic membrane can lead to middle ear infections as it allows many organisms to pass from the external ear to middle ear. Therefore, repairing this perforation is important in preventing such infections.
Endoscopic ear surgery has gained widespread application in the field of otology as a minimally invasive surgical technique that reduces patient morbidity.
In myringoplasty, traditional microscopic approach is one of the most frequently performed procedures. However, some disadvantages associated with this approach include limited visualization of surgical field, especially in cases of anterior quadrant or marginal perforation, as well as difficulty encountered due to the prominent anterior canal wall [1,2]. The endoscopic push-through perichondrial myringoplasty (EPPM) approach enables direct visualization of the entire eardrum and requires a minimal incision on the tragus for harvesting tragal perichondrium [3]. Thereby, it eliminates the need to perform canaloplasty or post-aural approaches to achieve a wide surgical view and eliminates the need for the elevation of tympanomeatal flap, which can potentially injure the ossicles, tympanic annulus, and chorda tympani and increase postoperative patient discomfort.
The present study evaluates the efficacy of EPPM without tympanomeatal flap elevation on the clinical and audiological outcomes in patients with chronic otitis media.
Subjects and Methods
Patients
We retrospectively reviewed the medical records of 40 patients with chronic otitis media who underwent EPPM without tympanomeatal flap elevation between July 2018 and January 2023. After excluding 6 patients who did not complete the minimum 3-month follow-up period, a total of 34 patients were included in this study. Patients who had cholesteatoma or otorrhea in the previous 3 months as well as those with near-total or total tympanic membrane perforation were excluded from this procedure. Patients with perforations located in the posterior quadrant of the tympanic membrane or involving the malleus were excluded from this procedure because these locations frequently require ossicular chain manipulation or reconstruction, which would introduce additional variables affecting audiological outcomes beyond the myringoplasty technique itself.
The size of tympanic membrane perforation was classified according to the percentage of the tympanic membrane area affected: small perforations were defined as those involving less than 25% of the total tympanic membrane area, moderate perforations as those involving 25%-50%, and large perforations as those involving more than 50% of the tympanic membrane area.
Operation technique
Surgery was performed under general or local anesthesia, depending on factors such as patient’s age, general status, and preference. The entire tympanic membrane was visualized using a 0° or 30°, 2.7×110 mm rigid endoscope. Topical anesthesia was administered using 2% lidocaine and 1:100000 epinephrine injections to the posterior, inferior, superior, and anterior walls of the external ear canal and tragal area. The margins of the perforation were trimmed using an angled pick and microforceps. An incision was made 2 mm posteriorly, running parallel to the free edge of the tragus. The tragal perichondrium and cartilage were dissected and harvested using curved iris scissors. The tragus incision site was sutured using the 4-0 Prolene® (Johnson & Johnson) sutures. The middle ear was tightly packed with Otopore® (Stryker) through the trimmed perforation, ensuring that it reached till the level of perforation. The harvested perichondrium graft was pushed through the perforation, and placed in the underlay position. Finally, the external auditory canal was packed with Otopore® and vaseline gauze. The surgical procedure is described in Fig. 1. All surgical procedures were performed by a single surgeon (E.P.), an otologist with over 2 years of experience in endoscopic ear surgery who had completed more than 30 endoscopic ear surgeries prior to this study period.
Surgical procedure and outcome of endoscopic push-through perichondrial myringoplasty without tympanomeatal flap elevation. Margins of tympanic membrane perforation (asterisk) are trimmed using angled pick, and malleus handle (arrow) is visible (A), middle ear cavity is packed with Otopore® until the level of perforation (B), perichondrium graft is placed under the tympanic membrane (C), and representative endoscopic image at 3-month follow-up showing completely healed tympanic membrane (D).
Outcomes analysis
Graft success rate, audiological outcomes, and surgical complications were assessed as primary outcomes. Graft success was defined as complete closure of the tympanic membrane without retraction, perforation, or atelectasis at the final follow-up examination (minimum 3 months post-surgery). All audiological evaluations were performed using standardized pure-tone audiometry (PTA). Air conduction (AC) thresholds were measured at 250, 500, 1000, 2000, 4000, and 8000 Hz, while bone conduction (BC) thresholds were measured at 500, 1000, 2000, and 4000 Hz. For calculating average hearing thresholds, we used the six-tone average method according to the Korean Audiological Society guidelines, which calculates the weighted average by multiplying the values at 500 Hz and 1000 Hz by 2, multiplying 2000 Hz by 2, adding the value at 4000 Hz, and then dividing the sum by 6. Airbone gap (ABG) was calculated as the difference between AC and BC thresholds using the same calculation method. Hearing success was defined as mean ABG closure to ≤20 dB at the final audiometric assessment.
Postoperative audiological assessments of seven patients were lost, resulting in the data from 26 patients being included in the analysis of pre- and postoperative audiological outcomes using the Wilcoxon signed ranks test, and results are presented as mean±standard deviation despite using nonparametric testing, as our data did not show severe skewness. Data were analyzed using the SPSS software, ver. 11.5 (SPSS Inc.), and a p-value of <0.05 was considered statistically significant. Other outcome analyses were performed in whole patients.
Postoperative care
Most patients were discharged on the same day of the surgery. They were instructed to avoid water or any other materials entering into the ear and were prescribed a systemic antibiotic and nonsteroidal anti-inflammatory drugs. The patients were routinely followed up at post-operative intervals of 1 week, 2 weeks, 6 weeks, and 3 months. Subsequent follow-up periods were determined based on the graft state. Sutures from the tragus incision were removed at the 1-week postoperative appointment, and packing material (Otopore®) was removed at 2 weeks. PTA was conducted 3 months postoperatively.
Ethics
Ethics Committee Approval for the study was obtained from the Institutional Review Board (IRB) of the Medical Center (IRB Number: 2022AN0485). All patients were informed of possible complications of surgery such as graft failure, temporary vertigo, etc. They all signed an informed consent form which is obtained from the IRB and consented to participate in the study.
Results
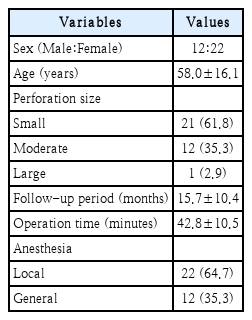
A total of 34 patients were enrolled in our analysis. Their demographic data are summarized in Table 1. The mean age of the patients was 58.0±16.1 years, ranging from 18 to 83 years. The size of the perforation was classified as small (61.8%), moderate (35.3%), and large (2.9%). Mean postoperative follow-up period ranged from 4 to 45 months, with a mean of 15.7±10.4 months. The average duration of operation was 42.8±10.5 minutes. Among these patients, 22 underwent surgery under local anesthesia and 12 under general anesthesia.
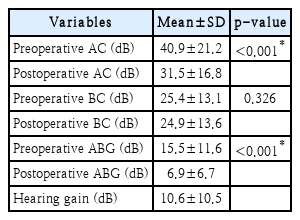
The mean AC threshold significantly decreased from 40.9 ±21.2 dB preoperatively to 31.5±16.8 dB postoperatively (p<0.001). The mean ABG showed a significant improvement from 15.5±11.6 dB preoperatively to 6.9±6.7 dB postoperatively (p<0.001), with a mean hearing gain of 10.6±10.5 dB. BC thresholds remained stable (25.4±13.1 dB preoperatively versus 24.9±13.6 dB postoperatively, p=0.326). Hearing results before and after surgery are summarized in Table 2. Hearing success rate, defined as the proportion of postoperative ABG ≤20 dB cases among total number of patients, was 92.3% (24/26).
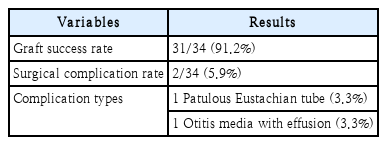
Graft success rate was estimated to be 91.2% (31/34). Among the three cases in which graft failure occurred, two cases had graft medialization, and one case had re-perforation due to graft erosion. Surgical complication rate was 5.9% (2/34). The complications included the patulous Eustachian tube and otitis media with effusion. Table 3 demonstrates the clinical outcomes of EPPM.
Discussion
Endoscopic transcanal myringoplasty cases have been reported since 1992 [4]. In recent years, the advantages of endoscopic tympanoplasty have become more prominent compared to those of traditional microscopic tympanoplasty. The endoscopic approach provides wide surgical views, including access to deep corner space, and it saves operation time because manipulation of magnification and focusing with the endoscope is faster and easier than with a microscope.
Additionally, EPPM offers a minimally invasive and fast surgical approach compared to endoscopic type I tympanoplasty, which requires the elevation of tympanomeatal flap [5].
Endoscopic butterfly-inlay myringoplasty (EBM) technique is an emerging approach similar to EPPM, which has a good graft success rate. However, the potential disadvantage of EBM, such as the risk of triggering cholesteatoma owing to its double-layered graft technique, remains a topic of controversy [6].
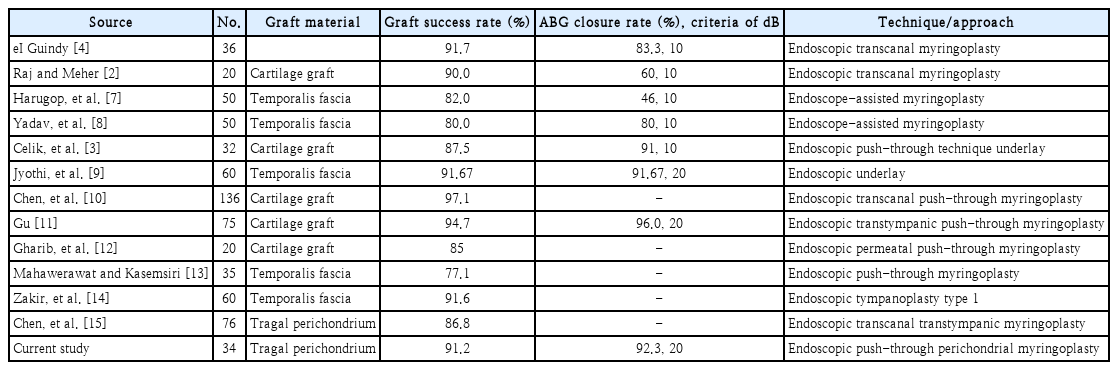
In our study, EPPM without tympanomeatal flap elevation was performed on 34 patients. Mean hearing gain, hearing success rate, and graft success rate were 11.6±10.8 dB, 92.3%, and 91.2%, respectively. Table 4 summarizes results from several studies that have analyzed the graft success rate and ABG closure rate in endoscopic assisted surgery. The graft materials used in the procedure included temporalis fascia, cartilage graft, and tragal perichondrium. The graft success rate has been reported to range from 77.1% to 97.1% [2-4,7-15]. The graft success rate of 91.2% is promising but slightly lower than some established techniques reporting success rates of 94.7%-97.1% with cartilage myringoplasty [8,9]. This difference may be attributed to our learning curve with the endoscopic approach and our inclusion of moderate and large perforations that might have been excluded from some comparative studies. However, the use of tragal perichondrium as graft material offers several advantages that likely contribute to our favorable outcomes. The perichondrium provides ideal thickness and pliability while maintaining excellent structural integrity and vascularization potential. The harvest technique is straightforward with minimal donor site morbidity compared to temporalis fascia. This graft material adapts well to various perforation sizes, though we acknowledge its potential limitations in near-total perforations where cartilage reinforcement may be preferable for structural support [13].
Despite the advantages of the endoscopic approach, it presents certain technical challenges worth acknowledging. The one-handed instrumentation technique required in endoscopic surgery can initially limit surgical maneuverability compared to bimanual microscopic approaches [14,15]. Additionally, the two-dimensional visualization sacrifices some depth perception. The learning curve for these adaptations should be considered when implementing this technique [7,14].
In our study, two surgical complications, including the patulous Eustachian tube and otitis media with effusion were noted. In the case of patulous Eustachian tube, the patient exhibited severe chronic obstructive pulmonary disorder, which had the potential to trigger cachexia. In the case of otitis media with effusion, the patient was on follow-up for nasopharyngeal cancer after receiving concurrent chemoradiotherapy. No other complications except these two special circumstances were noted.
While our study demonstrates promising results for EPPM, several limitations merit careful consideration. Our relatively small sample size of 34 patients, with only 26 available for detailed audiological analysis, constrains the statistical robustness of our findings and limits generalizability. As a single-center retrospective review, the study lacks a comparative control group, preventing definitive assessment of the technique’s superiority over traditional microscopic approaches. The moderate follow-up period of 15.7±10.4 months may not fully capture potential long-term surgical outcomes or late complications.
Strict patient selection criteria, while necessary for maintaining research integrity, simultaneously restrict the applicability of our findings to more complex middle ear pathologies. The loss of postoperative data for seven patients introduces potential bias in our hearing outcome analysis. And the technique’s reliance on specialized endoscopic skills and specific instrumentation presents a practical challenge for widespread adoption. Its reproducibility depends significantly on the surgical expertise and available equipment [5,15].
Future research should focus on multi-center prospective studies with larger, more diverse patient cohorts. Implementing randomized controlled designs that directly compare EPPM with traditional myringoplasty techniques would provide more definitive insights. Extended follow-up periods and more comprehensive patient protocols are essential for establishing the technique’s long-term clinical value.
Despite these limitations, our study offers valuable evidence of EPPM’s potential. The technique presents a promising minimally invasive approach to tympanic membrane reconstruction, with favorable surgical and audiological outcomes that warrant continued investigation. Its potential to reduce patient morbidity and improve surgical precision makes EPPM an important area of future otological research.
In conclusion, this study revealed that EPPM without tympanomeatal flap elevation is an effective surgical technique yielding favorable surgical and audiological outcomes in patients with chronic otitis media.
Notes
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2021R1I1A1A01052753), Ministry of Science and ICT (2022R1A4A1018869), and Korea University Research Fund (K2125741, K2211761). These funding sources provided only financial support and played no specific scientific role in this study.
Author Contribution
Conceptualization: Euyhyun Park. Data curation: Euyhyun Park. Formal analysis: Euyhyun Park. Funding acquisition: Euyhyun Park. Investigation: Euyhyun Park. Methodology: Euyhyun Park. Project administration: Euyhyun Park. Resources: Euyhyun Park. Supervision: Jiwon Chang, Gi Jung Im. Validation: Jiwon Chang, Gi Jung Im. Visualization: Soo Jeong Choi, Jiwon Chang, Gi Jung Im. Writing—original draft: Tae Hoon Lee. Writing—review & editing: Euyhyun Park.